in Foot and Ankle Surgery and Reconstruction
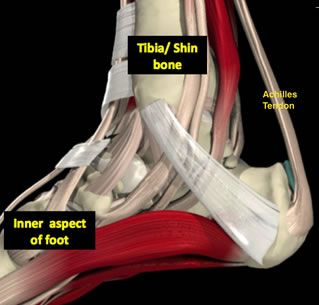
The Achilles tendon is the large, strong tendon that connects the calf muscles, specifically the gastrocnemius and soleus muscles to the heel bone or calcaneum. It allows you to point your foot downwards and push off the ground when you are walking or running.
The tendon is made up of strong fibres made of collagen. Over time this substance can “degenerate” and become weaker and less flexible. As this occurs then tiny microscopic tears can develop in the tendon, leading to weakness, pain and eventually swelling. The tendon swelling often develops in the middle of the tendon because this area has a less well-developed blood supply hence unable to heal itself effectively.
This is a commonly used term for anyone with Achilles pain. It is not strictly accurate, purely because if you looked at the tendon under a microscope there is tissue degeneration rather than inflammation of the tissue. It is more accurate to use the term “Achilles tendinopathy”.

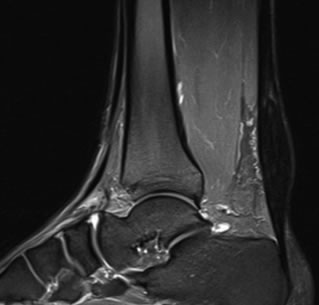
When pain, weakness and loss of function is associated with a swelling in the main portion of the tendon and not down at the bottom by the heel bone, it is referred to as Achilles tendinopathy. “Tendinopathy” is used to describe the typical microscopic findings in this condition and means tissue degeneration in the tendon fibres.
When pain, weakness and loss of function is associated with a swelling down at the bottom of the tendon by the heel bone, it is referred to as insertional Achilles tendinopathy. This is because the tendon “inserts” onto the heel bone. Sometimes the heel bone can be quite prominent here and very painful. This can be because of a combination of problems here including:

The clinical features usually diagnose the problem. An X-Ray can be done to look for tissue swelling or bone spurs. A more helpful test is an ultrasound which can easily be done to look at the tendon quality or an MRI.
People often “live” with the symptoms for quite a while, or alter their activity profile. The symptoms can unfortunately progress with a potential even for rupture of the tendon. It is advisable getting assessed by a foot and ankle surgeon or physiotherapist when possible.
Both insertional and non-insertional tendinopathy can be treated in a similar fashion.
The treatment is operative or non-operative.
The vast majority of patients require no surgery. Activity modification and rest coupled with suitable anti-inflammatories or pain-killers can really make a difference. Early rest in a boot may be needed in the short-term. A small heel raise (silicone insert) can help in the shoe. It is important to get introduced to a correct physiotherapy regime as they can prove hugely successful IF FOLLOWED AS INSTRUCTED. If physiotherapy is not fully successful then shock wave therapy can be used which has good results.
Operative treatment can be performed if other measures fail. Surgery usually involves exploration of the painful tendon area and removal of the degenerate/inflamed tissue or painful bony bumps on the heel. If the tendon is detached from the bone during surgery or a large amount of the tendon is removed then using another tendon in the foot to support the damaged Achilles tendon may be needed. This is not usually needed.