in Foot and Ankle Surgery and Reconstruction
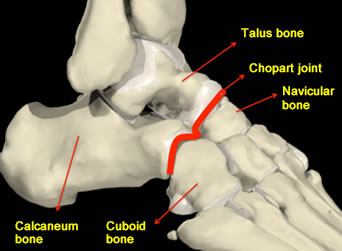
The hindfoot generally refers to the section of the foot that begins immediately below the ankle joint and ends at the level of the Chopart joint. You cannot feel the Chopart joint but it is made up of 2 joints in line, called the talonavicular joint and the calceneocuboid joint and is found below and in front of the ankle joint.
The hindfoot contains 2 main bones called the talus and the calcaneum (heel bone) that are connected by “joints” to one another and also these bones are connected in front to the “midfoot” area where the hindfoot meets the navicular and cuboid bones at the “Chopart joint”.
 There are different reasons for developing arthritis in the hindfoot:
There are different reasons for developing arthritis in the hindfoot:
 The clinical features as discussed above in addition to typical X-Ray findings seen can confirm the diagnosis. Further scans are usually unnecessary, but some surgeons will arrange a CT scan to exactly identify the joints involved.
The clinical features as discussed above in addition to typical X-Ray findings seen can confirm the diagnosis. Further scans are usually unnecessary, but some surgeons will arrange a CT scan to exactly identify the joints involved.
People often “live” with the symptoms for many years and then finally seek medical attention. If you decide not to see your doctor, the problem will tend to progress, usually slowly. Stiffness will usually increase and the pain can get worse making walking gradually more difficult and weight bearing exercise difficult. The condition can be treated at any stage but as it develops, the hindfoot can slowly move out of shape and affect other nearby joints with arthritis.
The treatment can involve a combination of different therapies below:
Surgery usually necessitates formal stiffening procedures of the arthritic joints involved. Depending on how many joints are affected one or all (there are 3) of the main joints can be part of a hindfoot fusion. This is a successful operation because the arthritic joints are already usually stiff and “painful” but following surgery although still stiff, they will be “painless”.
Many patients are simply seeking advice on managing a problem. In mild cases modifying shoes or activities can prove a successful therapy however if non-operative measures have failed to improve symptoms then surgery is indicated, but the timing of the surgery can be arranged to suit your needs. As said earlier, even if the condition worsens, surgery is always an option, but the exact surgical procedure performed may differ slightly from the original surgery possible and may be more technically challenging.