in Foot and Ankle Surgery and Reconstruction
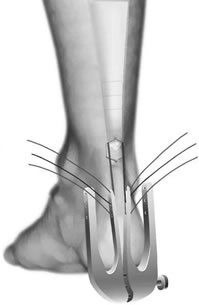
It is a daycase operation. The operation is done under a general anaesthesia and an added injection around the area to numb it after surgery. The operation involves a small incision (5cm) over the Achilles tendon, if done minimally invasively using the device below this still requires an incision, only smaller still. The procedure involves carefully reattaching the tendon ends with a strong suture that will not need to be removed later on. Dissolvable skin stitches may be used but your surgeon will inform you if not.
You will be given adequate pain relief medication. You will be in a below the knee plaster cast. Your physiotherapist will advise on mobility non-weight bearing on the leg during your stay. You will be discharged when you are comfortable and given a follow-up out-patient appointment.
The physiotherapist will follow the rehabilitation schedule on this website and guide you through the stages. It is vital that you adhere to the advice given to you. This schedule is only a guide and can vary between patients.
Keep the plaster cast totally dry. You may shower with a waterproof cover over the plaster. Once the plaster is removed you may shower if the wound is healed but gently dab the wound dry. Be careful not to stumble on the ankle out of the boot.
Once out of cast, do not pull at scabs but let them fall away naturally. If your wound becomes red, swollen or sore you need to see your Consultant to ensure there is no infection present. Your physiotherapist may advise on wound massage.
DVLA states it is the responsibility of the driver to ensure they are always in control of the vehicle. A good guide is if you can stamp down hard with the foot to stop the car in an emergency stop. This will take at least 10 weeks. Click here to read DVLA guidance.
This is very individual and job-dependent. Below is a guide:
Full range of movement to the ankle with normal power and function and full return to sports and previous activities. The timing of which can vary between individuals. Return to high level sports can take between 6 to 9 months, return to a more sedentary lifestyle between 4-6 months. Overall outcome is very good in the majority of patients with over 90-95% being very pleased.
Any operation carries a risk. Below is a guide to some risks potentially encountered. It is the surgeons duty to fully inform you of possible risks. Mr Roche will ensure this is always done so patients can make safe and informed choices about their operation.
If happens, in around 5%, it is usually simply treated with antibiotics. Significant consequences from infection are very rare but can be dealt with.
Nerves that supply sensation to the skin are near the incision site. Damage is rare but if your toe or outside of foot stays numb after surgery, the nerve may be bruised. If so it usually recovers. Risk is <5%.
Often due to a repeated injury or stumble. You will need to seek urgent medical attention to discuss whether re-operation is a good option. Re-rupture occurs in between 2-5%, but current “accelerated movement and weight-bearing rehabilitation” techniques may reduce the risk.
Symptomatic clot formation in the leg is unusual after Achilles surgery (2-5%). Some patients can develop clots that cause no problem whatsoever. Whether treatment to prevent clot is needed can be discussed with your surgeon. There is no consensus amongst UK Orthopaedic surgeons as to whether preventative medicine is needed.
This document is only meant to be a guideline to help you understand your treatment and what to expect. Every person is different and your rehabilitation may be quicker and slower. This will be advised and guided by your doctor and physiotherapist.
| Phase 1 | Protection (0-8 weeks) |
| Phase 2 | Early Mobilisation (6-12 weeks) |
| Phase 3 | Strengthening (12-20 weeks) |
| Phase 4 | Return to Activity (5-7 months) |
| Phase 5 | Return to play (8-12 months) |
| TREATMENT WEEK AND GOALS | TREATMENT PROCESS | |
| Week 1 • Rest and elevate the limb • Reduce Swelling and bruising • WB as advised |
Vacoped fixed on 30 ° with wedged sole. | Patient in Equinus (30° PF) POP. |
| Week 2 • Rest and elevate the limb • Reduce Swelling and bruising • WB as advised |
Consider even up shoe raise on the unaffected limb. Shower using the waterproof cover. |
|
|
Week 3 |
Vacoped fixed on 30 -25 ° with wedged sole, wear 24hrs. |
Gentle Soft tissue massage |
|
Week 4 |
Vacoped fixed 30-20 ° with wedged sole |
Introduce Passive and Active PF with Theraband Avoid any DF or stretches above neutral Increase gentle active exercises in PF position (Seated heel raises, peroneals, toe flexors, invertors of the ankle) ROM 0° DF maximum |
|
Week 5 |
Vacoped fixed 30-15° with wedged sole |
By week 5 start to regain slowly Full PF, INV, EV |
|
Week 6 |
Vacoped fixed 30-10° change to flat sole | |
|
Week 7 |
Vacoped fixed 30-5° keep flat sole | |
|
Week 8 |
Vacoped fixed 30-0° keep flat sole |
By Week 8 Start Proprioception/Balance work |
|
Week 9 |
Discard Vacoped change to flat shoe with 1cm heel lift for 4 weeks use Vacoped outdoor |
Gait re-education Ecc/Con loading (bilateral to single emphasis on Ecc phase) To start NWB aerobic- e.g. bike (push with heel not toes) |
|
Week 10 |
flat shoe with 1cm heel lift for 2/4 weeks. No Vacoped outdoors | |
|
Week 11 |
flat shoe with 1cm heel lift for 3/4 weeks | Gentle WB dorsiflexion stretch (Lunge position) be over cautious to avoid over stretching this phase of tendon remodelling |
|
Week 12 |
flat shoe with 1cm heel lift for 4/4 weeks | |
|
Weeks 13-20 |
WB in shoes without heel lift | Gentle return to Plyometrics to start forwards, backwards, directional, change of direction walking and progress as see fit |
| Week 16 onwards to RTS | • Normal gait pattern • Improving KTW 80% of other leg • Improving walking exercise tolerance • Single leg stance with good control for >10 seconds • Ankle ROM between 10° DF to 35° PF • Able to complete single leg heel raise • Able to return to running on flat surfaces at 5 months when have 70% strength of unaffected leg • Girth of calf 1/2cm of unaffected leg |
| Week 20 onwards | • Able to single leg calf raise • Able to horizontal single leg hop x 3 with 75% of unaffected leg • Able to vertical single leg hop75% of unaffected leg • Sprint with toe off phase of running gait • Education that it can take up to 1 year to return to normal preinjury level |