in Foot and Ankle Surgery and Reconstruction
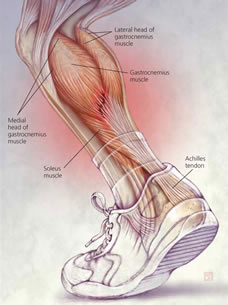
The Achilles tendon is the strong and large tendon found at the back of your ankle. It connects the calf muscle to the heel bone and is important in being able to bring the foot downwards, going on tip-toe and also providing a good push-off when walking or running.
This is a tear of the tendon. This may partial or complete. In complete ruptures there is complete loss of the connection between the muscles in the back of your calf and the heel bone.
Achilles ruptures are seen in about 1 in 5000 people. They are more common in men between the ages of 30-50.
As any material, the tendon can be torn if a great force goes through it. This can be after a fall, but usually happens in sports when a sudden force from the calf muscles puts too much stress through the tendon. This often happens when the tendon is not accustomed to such force, for example in people trying to train too quickly and too hard and/or when the tendon may be weak. Factors such as ageing, the long-term use of corticosteroids, steroid injections near the tendon and certain antibiotics (e.g. ciprofloxacin) can all weaken the Achilles tendon over time.
When the tendon ruptures, one will usually experience a sudden pain at the back of the ankle (like being hit there with a bat) and may hear a snap. Afterwards one will find it difficult to walk and push the foot off the ground. The gap of the torn tendon may be felt, whilst swelling and bruising may develop soon after.
Pain afterwards may surprisingly be minimal. If you think you may have torn your Achilles tendon it is better to get it checked sooner rather than later because early appropriate treatment will give you a better outcome.
Usually a patient history of events and clinical examination confirms the diagnosis. Sometimes, an ultrasound or rarely an MRI scan is performed to confirm the diagnosis for example when there is uncertainty.
If you have NO treatment at all, not even a rigid boot or plaster, the tendon may heal elongated causing weakness in the calf muscles and difficulty in walking and certainly running. It is advisable that you receive some treatment, which may be either non-operative or operative. There is still some controversy about what is the best choice, and the decision will be based on a discussion between yourself and your doctor about the pros and cons of each. Decisions will depend on your general health and activity level, as well as the exact site of and extend of the rupture.
With non-operative treatment the tendon heals naturally, by keeping its two torn ends close together in a plaster cast or a brace. As long as the two end of your torn Achilles tendon are close together they will re-attach to each other naturally. This is why its vital the appropriate plaster/boot is used as soon after the injury as possible so the tendon heals at its correct length.
Please refer to the Rehabilitation Guidelines after Acute Achilles Tendon Rupture - NON-OPERATIVE TREATMENT for an accurate schedule. It is important to appreciate the exercise schedule is a guide and patients will vary.
It is essential that you elevate your ankle as much as possible for the first two weeks as this will help with the pain and swelling.
You will be in a cast or boot for the first two weeks and no weight must be put through the leg. You must use crutches and keep the foot elevated as much as possible. You will then be allowed to put your weight through your leg after 2 weeks. Your recovery process will be supervised by the physiotherapist who will guide you through the rehabilitation. It is vital you adhere to the advice to ensure good progress.
A good guide is if you can stamp down hard with the foot to stop the car with the brake, such as is needed in an emergency stop. This will be when the boot is removed so around 10 weeks.
This is very individual and job-dependent. Below is a guide:
With surgical treatment, the two torn ends are brought together and held together with sutures until they heal. This is done with a very small incision. Different techniques can be used and different incisions. Rehabilitation in a brace will follow.
Please refer to the Operation page on Achilles Tendon repair.
Please refer to the Rehabilitation Guidelines after Acute Achilles Tendon Rupture - OPERATIVE TREATMENT for an accurate schedule.
There is a potential risk of developing a clot in the calf (deep vein thrombosis) after either treatment. To minimise this arrangements can be made for you to receive a blood-thinning drug (usually injections) to protect you. This can be discussed with the doctor.